
SYMPTOMS OF BRADYCARDIA
When your heart beats too slowly, you may experience various symptoms. These symptoms help your doctor assess the severity of your heart condition and determine the appropriate treatment for you.
- Dizziness and fainting
- Chronic lack of energy
- Shortness of breath
![]()
![]()
![]()
CAUSES OF BRADYCARDIA
Bradycardia can occur for several reasons. Some common causes of bradycardia include:
- Congenital heart disease (condition you were born with)
- Certain illnesses or heart medications
- Natural aging process
- Scar tissue from a heart attack
- Sick sinus syndrome, also called sinus node dysfunction (the heart’s natural pacemaker is not working correctly)
- Heart block (the electrical impulse that travels from the upper to the lower chamber of the heart is irregular or blocked)
DIAGNOSIS OF BRADYCARDIA
Only your doctor can determine if you have bradycardia and, if so, how far it has progressed. To rule out or confirm the diagnosis of bradycardia, one or several diagnostic tests may be ordered, depending on the suspected heart rhythm problem.
These may include:
- Electrocardiogram (ECG)
- Exercise ECG, or stress test (measures your heart rhythm while you’re engaged in a physical activity)
- Holter or event monitor
- External loop recorder
- Insertable cardiac monitor
- Tilt table test
- Electrophysiology study (EP study)
TREATMENT OF BRADYCARDIA
How bradycardia is treated depends on what’s causing it. Bradycardia can be caused by an underactive thyroid (hypothyroidism), an electrolyte imbalance, or medicines you may be taking for certain conditions. Treating these problems with new medicines, or adjusting the doses of the medicines you are currently taking, may restore a normal heartbeat. If treating these problems medically doesn’t work, or if damage to the heart’s electrical system causes your heart to beat too slowly, then you may be prescribed a pacemaker
WHAT IS A PACEMAKER?
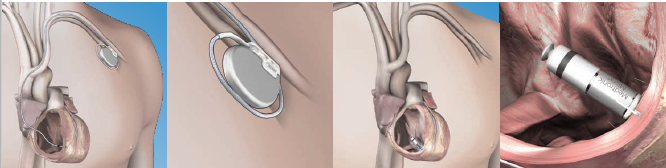
When people refer to a pacemaker, they are actually discussing a pacing system, which includes the pacemaker and leads.
- A traditional pacemaker is a small device that is implanted under the skin, typically just below the collarbone. The device delivers therapies to treat irregular, interrupted or slow heartbeats
- Leads are thin, soft, insulated wires about the size of a spaghetti noodle. The leads carry the electrical impulse from the pacemaker to your heart and relays information about the heart’s natural activity back to your pacemaker

Recently leadless pacemakers. Unlike traditional pacemakers that are placed in the chest with leads running to the heart, they are implanted directly into the heart via a vein in the leg and are completely self-contained within the heart
HOW DOES THE PACEMAKER WORK?
A pacemaker is designed to mimic the heart’s natural rhythm when there are disturbances, such as pauses in the natural rhythm. The pacemaker has two main purposes — pacing and sensing.
Pacing - A pacemaker will send an electrical impulse to the heart when the heart’s own rhythm is too slow or is interrupted. This electrical impulse starts a heartbeat.
Sensing - A pacemaker will also “sense” (monitor) the heart’s natural electrical activity. When the pacemaker senses a natural heartbeat, it will not deliver a pacing pulse.
THE PACEMAKER BATTERY
The energy needed for the pacemaker to work comes from a battery inside the pacemaker. How long your battery lasts depends on several factors. Some of these factors include the type of pacemaker you have, the nature of your heart condition, and how often your pacemaker provides therapy to your heart.
The battery could last over 13 years. Because your pacemaker operates using a battery sealed inside the device, the entire device will need to be replaced when battery power falls to a low level. The leads only need to be changed in exceptional cases.
GETTING A PACEMAKER IMPLANTED
The procedure to implant a pacemaker does not require open heart surgery, and most people go home within 24 hours. Before the surgery, medication may be given to make you sleepy and comfortable. Generally, the procedure is performed under local anesthesia.
GENERAL STEPS OF AN IMPLANT PROCEDURE:
- A small incision, approximately 5 to 10cm long, will be made in your upper chest area, just below your collarbone
- One or two leads will be guided through a vein into your heart, and the leads will be connected to the pacemaker
- Single chamber pacemakers mean one lead is inserted either into the lower right chamber (ventricle) of the heart or into the upper right chamber (atrium) of the heart
- Dual chamber pacemakers mean one lead is inserted into the upper right chamber (atrium) of the heart and one lead into the lower right chamber (ventricle) of the heart
- The pacemaker settings will be programmed, and the device will be tested to ensure it is working properly to meet your medical needs
- The pacemaker will be inserted beneath your skin, and the incision in your chest will be closed
REPLACEMENT PROCEDURE
The pacemaker has been developed to let your doctor know when the battery power falls to a low level. As the battery is an inherent component of the pacemaker, the entire pacemaker must be replaced during a replacement procedure. The surgeon makes an incision over the old scar and removes the old device. The electrodes are fastened securely and, after they have been checked, a new device is connected, tested, and inserted into the existing skin pocket. The leads only need to be changed in exceptional cases.
LEADLESS PACEMAKER
The leadless pacemaker is 93% smaller than traditional pacemakers. It is comparable to the size of a large vitamin capsule and has a battery that typically lasts between 8 and 13 years.
Unlike a standard pacemaker, the leadless pacemaker is implanted into the heart through a vein in your groin and does not require a pacing lead. The miniaturized size and minimally invasive approach leaves no visible sign of a medical device under the skin. This means fewer post-implant activity restrictions and no limitations on shoulder movement.
IS IT SUITABLE FOR ALL PATIENTS?
The leadless pacemaker is intended for patients with specific pacing needs. Ask your doctor if it is an option for you.
HOW IS A TRADITIONAL PACEMAKER SYSTEM IMPLANTED?
A small incision, approximately 5 cm long, is made in the upper chest.
A lead (thin insulated wire, like a spaghetti noodle) is guided through the vein into the heart.
Your doctor connects the lead to the pacemaker and programs the device.
The pacemaker is then inserted beneath the skin.
Your doctor tests the pacemaker to ensure it is working properly.
The incision is then closed with stitches.
HOW IS THE LEADLESS PACEMAKER IMPLANTED?
Your doctor will insert a thin catheter system into a vein, typically near the upper thigh. The catheter system moves the pacemaker into the right ventricle of the heart. The pacemaker is placed against the heart wall and secured with flexible tines (see image below). Your doctor tests the pacemaker to ensure it is working properly. The catheter system is then removed.
REPLACEMENT PROCEDURE
A new Leadless Pacemaker is needed when battery power falls to a low level. Battery power is affected by many factors, including the nature of the heart condition.
The estimated average battery life for a Leadless Pacemaker device is approximately 8-13 years after it is implanted. Individual patient experience may vary. The battery power is checked at each pacemaker’s follow-up appointment. The doctor or nurse will notify you when you need a new pacemaker. When a new device is needed, the device may be either simply turned off or removed from the body before a new device or traditional pacemaker system is implanted. Your doctor will determine what is best for you.
FOLLOW-UP CARE AND MONITORING
Your doctor will set follow-up appointments. During such follow-ups, you should not only mention the symptoms that may have occurred during the action of the pacemaker, but you should also take this opportunity to ask any questions you may have and talk about your concerns and potential fears.
The follow-up appointments enable your pacemaker to be thoroughly checked. During these check-ups, your doctor may:
Monitor the battery status of the Pacemaker
Review and adjust (if needed) your Pacemaker settings to ensure they are programmed appropriately for your medical needs
This is done through a programmer, a small computer kept at your doctor’s office. Your doctor will use the programmer to retrieve information stored in your Pacemaker.
REMOTE PACEMAKER MONITORING
We understand it is important to stay connected to your care team from the comfort of your home or wherever you’re traveling — remote monitoring allows for this flexibility.
Today, millions of people implanted with heart devices are remotely monitored. Remote monitoring has been shown to:
- Communicate any heart rhythm and device changes which require attention
- Reduce hospitalizations and Emergency Room (ER) visits
- Increase Quality of Life
- Provide you with a sense of security and peace of mind

