
SYNCOPE
On this page we will describe the definition of syncope, the different types it manifests and the causes that cause it. Finally, we will refer to various ways of dealing with syncope depending on its type
What is syncope?
By the term Syncopation we mean the oss of Consciousness n which:
-
There is total loss of Consciousness.
-
The patient cannot maintain an upright position and falls.
-
The symptom is transient, appears suddenly and lasts a short time(usually seconds)
-
There is automatic and full recovery.
It is important to use the term Syncope only if the patient exhibits all the above characteristics. Otherwise, the term loss of consciousness is more appropriate as it includes diseases that look like but are not Syncope.
The term Presyncope is used when the symptoms are like those of Syncope but do not lead to a complete loss of consciousness although they have the same mechanism as it.
Pathophysiological, Syncope is due to a transient reduced blood supply to the brain.
Types and Causes of Syncope:
- Reflex (Neurocardiogenic) Syncope occurs when a Neurogenic (reflex) mechanism is involved either through the Vagus Nerve (Vagus Nerve, Vasovagal Syncope through the Bezold-Jarisch reflex) or throughother nerves and receptors of the human body, after certain stimuli. These can be normal events such as prolonged standing or even events such as laughing, urinating or even pressure at the base of the throat in some sensitive individuals. Syncope of this type is considered the most benign and occurs in young and healthy individuals. During the episode the patient may have a slow pulse or long cardiac pauses bradycardia/asystole, cardio-inhibitory form) or low blood pressure (vaso-suppressive form) or both (mixed form). Reflex (mainly Vasovagal) Syncope is the most common form of syncope in all ages. It is important to be aware that multiple mechanisms may contribute to a Syncope episode, especially in the elderly. For example, dehydration can worsen susceptibility to reflex syncope, and so on.
- Vasovagal
- Orthostatic Vasovagal: standing, less often in a sitting position.
- After emotion: fear, Pain (Physical or visceral), catheterization, fear of blood
- Occasional
- After urination, gastrointestinal irritation (swallowing, defecation), coughing, sneezing, other (i.e. laughing, playing wind instruments)
- After exercise
- Carotid sinus syndrome
- Atypical Forms (Without precursor symptoms and/or triggering stimuli and/or with atypical symptoms)
There are 2 pathophysiological mechanisms for neurocardiogenic syncope:
1. Vaso suppression: Hypotension is due to insufficient vasoconstriction by the sympathetic system.
2. Cardiac arrest: Bradycardia or asystole due to predominance of the parasympathetic system.
- Cardiac (Cardiogenic) Syncope is the result of either an arrhythmia (Bradycardia or Tachycardia) or because of a structural disease of the heart (e.g. coronary artery disease, heart muscle diseases). By analogy, diseases of the lungs and great vessels such as pulmonary embolism and pulmonary hypertension can cause cardiac syncope. Syncope due to cardiac causes is the most serious of the other forms of Syncope and understandably carries the worst prognosis. It's second most common form is cardiac syncope which is extremely rare in children, teenagers, and young adults. It is estimated that the finding of cardiac causes of syncope doubles the risk of death and has a 6-month mortality 6-month mortality.
- Arrhythmia as Primary Cause:
- Bradycardia: sinus node dysfunction including bradycardia tachycardia syndrome, diseases of the excitatory system
- Tachycardia: Supraventricular, Ventricular
- Structural Heart Diseases:
- Aortic valve stenosis, acute myocardial infarction/myocardial ischemia, hypertrophic cardiomyopathy, cardiac masses (atrial myxoma, heart tumors), pericardial disease/ tamponade, congenital coronary artery disease, prosthetic valve dysfunction, etc.
- Cardiopulmonary causes and large vessels:
- Pulmonary Embolism, acute aortic dissection, pulmonary hypertension
- Orthostatic Syncope, we have when the decrease in cerebral perfusion is due either to a decrease in blood volume (hemorrhage, dehydration) or to an inability of the nervous system to maintain a stable and balanced tone and diameter of the vessels (neurogenic hypotension, primary or secondary) or due to drugs that affect vascular tone or blood volume. Orthostatic syncope is common in very elderly patients, but the medical history may be less reliable than in young patients.
- Medicines (the most common cause of OU): e.g. vasodilators, diuretics, phenothiazines, antidepressants
- Vascular volume reduction: bleeding, diarrhea, vomiting, etc.
- Primary Autonomic Nervous System (NEU): primary autonomic failure, systemic multiple atrophy, Parkinson's disease, dementia with Lewy bodies
- Secondary Autonomic Failure (Neurogenic OU): Diabetes, amyloidosis, spinal cord injuries, autoimmune autonomic neuropathy, paraneoplastic autonomic neuropathy, renal failure
Note: Hypotension may be aggravated by venous pooling during exercise, after meals, and after prolonged recumbency.
What symptoms can occur during Syncope / Pre-syncope?
In pre-syncope (prevented loss of consciousness) or shortly before syncope (Loss of Consciousness), the patient may subsequently describe the following:
- Darkening of the visual field
- Feeling "empty"
- Lethargy
- Fatigue
- Fainting after exercise or after certain stimuli such as coughing, laughing, swallowing, urinating, or defecating
- Loss of balance or weakness in standing
- Changes in vision (spots or tunnel vision)
- Feeling of Pulses
- Jaundice, sweating
- Hearing disorders: hearing loss, tinnitus, crackling sounds as if from a distance
- Headache
The above are described with the term prodromal symptoms and many of them are due to the activation of the Autonomic Nervous System.
During syncope, the patient may also present (as described by witnesses) abnormal epilepsy-like movements and loss of sphincter control (unlike epilepsy, these movements are irregular in range of motion, asynchronous, and asymmetric, and begin after losing consciousness).
How can benign syncope like vasovagal syncope affect my life?
Syncope due to cardiac causes is associated with increased mortality and hospitalizations compared to other forms of syncope. On the other hand, reflex syncope is benign and has an excellent prognosis.
It is estimated that one in four people will have at least one episode of Vasovagal Syncope in their lifetime, only 1 in 20 will have at least 5 in their lifetime and even fewer will have more.
Nevertheless, reflex syncope remains a serious health problem (when recurrent) as it is associated with a reduced quality of life. Patients with this type of Syncope, although not at risk of "immediate" death, may be injured during the syncope episode. This is especially important when there are no precursor symptoms. Eventually, recurrent reflex syncope can lead to interruption of activities such as school, work, recreation, or driving. These unwanted effects, in some people, can lead to psychological burden or even secondary depression.
When should I run for help?
The investigation of Syncope can only be done by specialized personnel. But there are some features that should prompt the patient to seek medical help quickly as they may be due to cardiac syncope.
- Syncope during exercise or in a supine or sitting position
- Sudden onset of pulse followed immediately by Syncope
- Presence of a family history of unexplained sudden death at a young age
- Known history of structural heart disease or coronary artery disease
- Known abnormal electrocardiogram
The absence of warning symptoms before syncope can be a characteristic (but not necessarily) of cardiac Syncope.
Syncope detection diagnostic options
- Cardiogram (ECG)
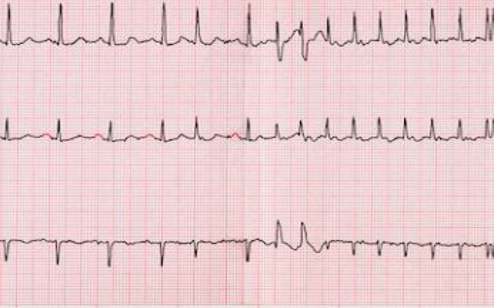
An ECG is a simple, painless test that records the heart's electrical activity. It is the most useful test for diagnosing atrial fibrillation. The ECG records the frequency of the heart's action and also the heart's rhythm (rhythmic or irregular activity). However, the ECG only records electrical activity for a few seconds. Thus, patients who at that time do not have atrial fibrillation cannot be immediately diagnosed. In patients with paroxysmal atrial fibrillation, which is intermittent in nature, the diagnosis can be made with continuous heart rate monitoring (Holter) devices.
- Holter
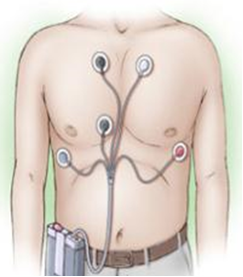
The Holter recorder records heart activity over a period of 24 hours, 48 hours, or sometimes longer intervals of days. Adhesive electrodes are attached to the patient in specific places on the chest. The electrodes are attached to a small portable recording device. The device is attached to the belt or worn as a necklace around the neck. It is preferred that the device be applied, and the patient continue with their normal daily activities.
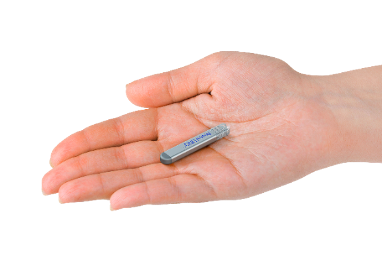
- Implantable Cardiac Monitoring Devices (ICM–ILR)
Implantable (injectable) rhythm monitoring devices (or ILR Implantable loop recorder or Implantable Cardiac Monitor ICM) are tiny devices (volume <1.5cc) compatible with MRI scanner (at 1.5 and 3.0 Tesla) that are implanted through a very tiny incision under the patient's skin and continuously record the ECG. They work with a battery that lasts 3-4 years and can be controlled either with an external programmer or with a remote patient monitoring device by the doctor, so that any recorded arrhythmia can be retrieved from their memory.
These devices are used when the arrhythmias under investigation are infrequent enough to be recorded during a 24-hour Holter. When the device's battery runs out or when the diagnosis is made, they can be removed.

How to deal with "benign" Syncope (Vasovagal/Orthostatic Syncope)?
Ideally, the investigation and treatment of Syncope should be done by specialized staff, doctors, and nurses, and preferably in a Syncope clinic. The initial assessment should aim to classify the syncope episode into one of the three categories of Syncope. Cardiac Syncope should be treated according to the underlying pathology and under medical supervision. Reversible causes of orthostatic hypotension (modification of medication, hydration, treatment of the underlying neurological disease) should be treated in the same way. However, there is a significant number of patients who either have benign reflex syncope or, after initial evaluation, remain as patients with syncope of unknown reason.
Reflex syncope is a major health concern not because of its low mortality but because of its recurrence and the risk of injury, especially when prognostic symptoms are absent.
Precautionary measures
Episodes of Vasovagal/Reflex Syncope can be predicted by:
- Educating the patient to recognize the precursor symptoms and prevent Syncope. Also, with reassurance of the benign nature of his/her symptoms.
- Avoidance of stimuli that cause syncope, such as prolonged standing, fear, or more specifically reflexes when a specific reflex intervenes, such as in syncope during urination.
- Adequate hydration and avoidance of hypotensive medications
- Manipulations to increase muscle tone (Counterpressure maneuvers - see image) / Compression socks
- Medicines that increase the pressure in certain cases
- Pacemakers, although more commonly used in previous years, are now a treatment option in a very limited population of patients with reflex syncope
There is broad agreement that education and lifestyle changes are highly effective in reducing recurrences of Vasovagal syncope. It is estimated that >50% do not have recurrences over the next 1 or 2 years, and in those who do reoccur, episode density is reduced by >70%. (source Guidelines of the European Society of Cardiology).
Measures to avoid an impending episode of Reflex Syncope
- When you feel the symptoms of Syncope coming on, the best reaction is to lie on the ground. If this is not possible, then sit down and perform manipulations to increase muscle tone. The final symptom is the blackout of the vision: when it appears, you will have only a few seconds to prevent fainting.
- Your doctor has shown you how to perform the manipulations to increase muscle tone. All these manipulations involve the "tightening" of large muscles of the body. One way is to squeeze the buttocks together and forcefully straighten the knees. Another way is to "cross" the lower limbs and exert pressure along their entire length. Also, clench your hands into fists and tense your upper limbs.
- Drink about 2 liters of fluids a day and do not use low-salt drinks unless there is a medical reason. A simple way to assess whether your hydration is sufficient is the color of your urine: If it is dark yellow, then there is less fluid in your body, so by taking extra water, try to keep it very lightly colored.
- Inform your immediate environment about what to do during a crisis: in a typical crisis, there is no need to call a doctor or an ambulance.

How to deal with Cardiac (Cardiogenic) Syncope?
Cardiac (Cardiogenic) Syncope cannot be treated with lifestyle changes, training in exercises, etc., because the risks to the patient's life are particularly high and there must be an invasive approach.
Depending on the cause of the syncope—bradycardia or tachycardia—the placement of a device that will "correct" the irregular way the heart beats with the goal of eliminating the symptoms is indicated.
If the patient suffers from some causes that lead to bradycardia (sick sinus syndrome or atrioventricular block), the recommended solution is the implantation of a pacemaker. On the contrary, when the causes lead to tachycardia (structural heart diseases, ventricular arrhythmias), then a defibrillator must be placed IMMEDIATELY.
WHAT IS A PACEMAKER?
When people refer to a pacemaker, they are actually discussing a pacing system, which includes the pacemaker and leads.
- A traditional pacemaker is a small device that is implanted under the skin, typically just below the collarbone. The device delivers therapies to treat irregular, interrupted, or slow heartbeats.
- Leads are thin, soft, insulated wires about the size of a spaghetti noodle. The leads carry the electrical impulse from the pacemaker to your heart and relay information about the heart’s natural activity back to the pacemaker.
Recently, leadless pacemakers have been developed. Unlike traditional pacemakers that are placed in the chest with leads running to the heart, they are implanted directly into the heart via a vein in the leg and are completely self-contained within the heart.
Leadless Pacemaker
Leadless pacemaker is 93% smaller than traditional pacemakers . It is comparable to the size of a large vitamin capsule and has a battery that typically lasts between 8 and 13 years.

Unlike a standard pacemaker, leadless pacemaker is implanted into the heart through a vein in your groin and does not require a lead. Miniaturized size and minimally invasive approach leaves no visible sign of a medical device under the skin. This can mean fewer post-implant activity restrictions and no obstructions to shoulder movement.
IS THE LEADLESS PACEMAKER SUITABLE FOR ALL PATIENTS?
The leadless pacemaker is intended for patients with specific pacing needs. Ask your doctor if the leadless pacemaker is an option for you.
WHAT IS AN ICD?
When people refer to an implantable cardioverter defibrillator (ICD), they are actually discussing the system: the defibrillator and the leads.
- A pulse generator (defibrillator) works like a small computer, continuously monitoring the heart and automatically delivering electrical pulses or shocks to correct fast heart rhythms. It is a small device about the size of a matchbox and is usually inserted just under the collarbone.
- Leads are thin, soft, insulated wires about the size of a spaghetti noodle. They are placed in your heart through a vein and connected to the defibrillator. The leads carry the electrical impulse from the defibrillator to your heart and relay information about the heart’s natural activity back to the defibrillator.
HOW DOES AN ICD WORK?
An implantable cardioverter defibrillator is designed to monitor your heart rhythm 24 hours a day. If your heart is beating too fast or irregularly, the device will first send small painless electrical signals to correct your heart rate (this is called anti-tachycardia pacing or ATP). If the fast heart rate (tachycardia) continues, the defibrillator will deliver an electric shock to restore your heart to a normal rate. This electric shock is synchronized with the heart’s rhythm as far as possible and is then referred to as cardioversion. If the electric shock cannot be synchronized with the heart’s rhythm, e.g., during ventricular fibrillation, it is referred to as defibrillation.
The implantable cardioverter defibrillator can also treat slow heart rhythms by sending electrical pulses to the heart to correct it.
Your doctor will program the ICD to deliver the most effective therapies for your specific heart condition.
What is the difference between a traditional ICD and an EV-ICD?
ICDs and EV-ICDs both have a defibrillator and a lead.
The defibrillator is a small computer that continuously monitors your heart rate. If it detects that your heart is beating too fast, it automatically sends electrical signals or shocks to restore a normal heartbeat. The defibrillator is about the size of a matchbox. A traditional ICD is placed just under your collarbone, while an EV-ICD is inserted under the left armpit.
The lead is a thin, soft, insulated wire about the size of a spaghetti noodle, which transmits electrical signals from your heart to the defibrillator, allowing it to monitor your heart. It also delivers treatments from the defibrillator to your heart. With a traditional ICD, the lead is placed in your heart through a vein. With an EV-ICD, the lead is placed under the sternum, outside the heart.
How does an EV-ICD work?
The EV-ICD is designed to monitor your heart rhythm 24 hours a day. If your heart beats too fast or irregularly, the device will first send small painless electrical signals to correct your heart rate (this is called anti-tachycardia pacing or ATP). If the fast heart rate continues, the defibrillator will deliver an electric shock to restore a normal heart rhythm. This electric shock is called cardioversion or defibrillation.
The EV-ICD can also treat slow heart rates by sending electrical pulses to the heart to correct it. Your doctor will program the EV-ICD to provide the most effective therapies for your specific heart condition.

