
WHAT IS HEART FAILURE?
The term heart failure does not mean your heart has stopped pumping, but rather that your heart muscle is not able to pump enough blood to meet your body’s needs.
As a result, you may feel tired, lack energy, experience shortness of breath, and notice excess fluid collecting in your body.
In a healthy heart, each chamber contracts (squeezes) in a coordinated effort. If the heart is not beating in a coordinated fashion, then the body will not receive an adequate amount of blood to function properly. During heart failure, the heart attempts to compensate for lost pumping power, which may change its shape and result in an uncoordinated (or unsynchronized) and inefficient heartbeat.
SYMPTOMS OF HEART FAILURE
Heart failure is a progressive condition, meaning it will gradually worsen. At first, you might not experience any symptoms, but over time your heart’s pumping ability will continue to weaken and you may experience some or all of the following symptoms:
- Chronic lack of energy
- Shortness of breath
- Swelling of feet and legs
- Swollen or tender abdomen with loss of appetite
- Difficulty sleeping at night due to breathing problems
- Increased urination at night
- Confusion and/or impaired memory
- Cough with frothy sputum
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
CAUSES OF HEART FAILURE
Heart failure usually develops slowly after an injury to the heart. There is no single cause, and sometimes the cause is unknown.
Some of the most common causes of heart failure are:
- Previous heart attack (myocardial infarction)
- Coronary artery disease
- High blood pressure (hypertension)
- Heart valve disease
- Infection of the heart (myocarditis)
- Congenital heart disease (condition you were born with)
- Endocarditis (infection of the heart’s inner lining)
- Diabetes (the body does not produce or properly use insulin)
RISK OF A POORLY PUMPING HEART:
In heart failure, the heart muscle must work harder to pump blood to the body. This may cause the heart to beat faster, which can lead to dangerously fast or irregular heart rhythms. These abnormal heart rhythms can lead to a condition called Sudden Cardiac Arrest (SCA).
WHAT IS SUDDEN CARDIAC ARREST?
Sudden Cardiac Arrest (SCA) results from an electrical problem with the heart that triggers a dangerously fast heart rhythm (ventricular fibrillation). The rapid, irregular heart rhythm causes the heart to quiver rather than contract or pump. When the heart stops pumping blood, oxygen cannot reach the body and brain. If not treated immediately, SCA can be fatal. Sudden cardiac arrest is one of the top killers and claims more lives than breast cancer, AIDS, or lung cancer.
HEART ATTACK AND SUDDEN CARDIAC ARREST: WHAT ARE THE DIFFERENCES?
Sudden cardiac arrest is not the same as a heart attack, although the two are often confused
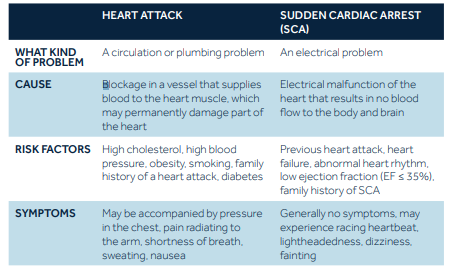
WHO IS AT RISK OF SUDDEN CARDIAC ARREST?
Generally, sudden cardiac arrest strikes without warning.
People who are at a higher risk for sudden cardiac arrest include:
- Those who have had a heart attack
- People who have heart failure
- Survivors of a previous sudden cardiac arrest or those who have a family member who has had a sudden cardiac arrest event
- People with a low ejection fraction (EF)
KNOW YOUR EJECTION FRACTION (EF)
EF - or Ejection Fraction - is the percentage of blood that is pumped out of your heart with each heartbeat. Your doctor uses your EF number to determine how well your heart is pumping. It can change over time, so it is important for you and your doctor to check your EF number regularly.
The most common way to measure EF is with an echocardiogram. This test is usually performed in a doctor’s office or hospital’s diagnostic area.
Chart of typical EF ranges:
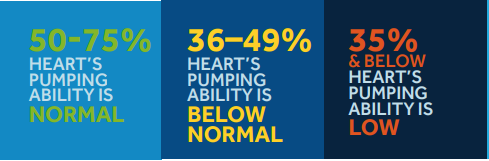
A healthy heart has an ejection fraction (EF) between 50% and 75%. This indicates the heart is pumping well and able to deliver enough blood to the body and brain. Even a healthy heart does not pump 100% of the blood out of the heart during each beat—some blood always remains in the heart.
People with a low EF (35% or below) are at an increased risk for sudden cardiac arrest (SCA).
Sudden cardiac arrest causes around 20% of all deaths in Europe.
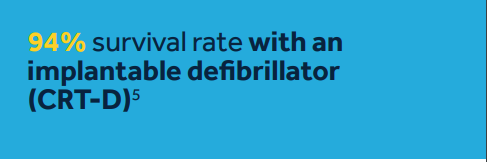
The most effective way to treat sudden cardiac arrest is through defibrillation. Defibrillation involves delivering an electrical shock to your heart to restore a normal heartbeat.
There are two primary forms of defibrillation:
- An automated external defibrillator (AED) is a portable device that is used by emergency response teams or the general public to shock the heart.
- An implantable heart device (called ICD or CRT-D) that is implanted under the skin. The implantable heart device delivers electrical pulses or shocks to treat fast, irregular rhythms.
TREATMENT OF HEART FAILURE
Heart failure is a progressive condition. Your doctor may prescribe a variety of treatment options that may slow the progression of the disease, strengthen your heart, and improve your quality of life. Some of these treatments may include medications, lifestyle changes, exercise, device therapy, or a combination of these.
WHAT IS A CARDIAC RESYNCHRONIZATION THERAPY (CRT) DEVICE?
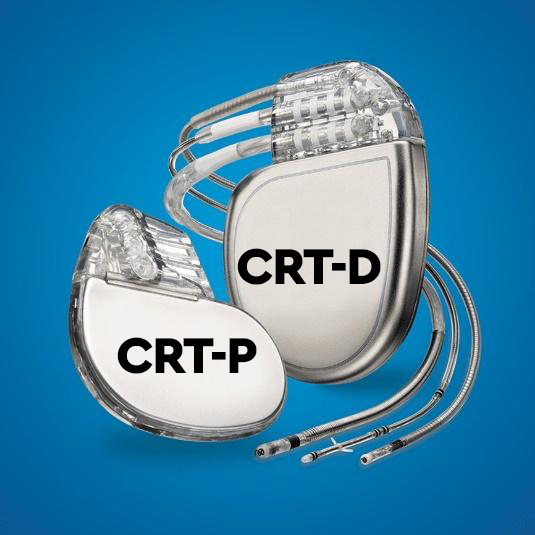
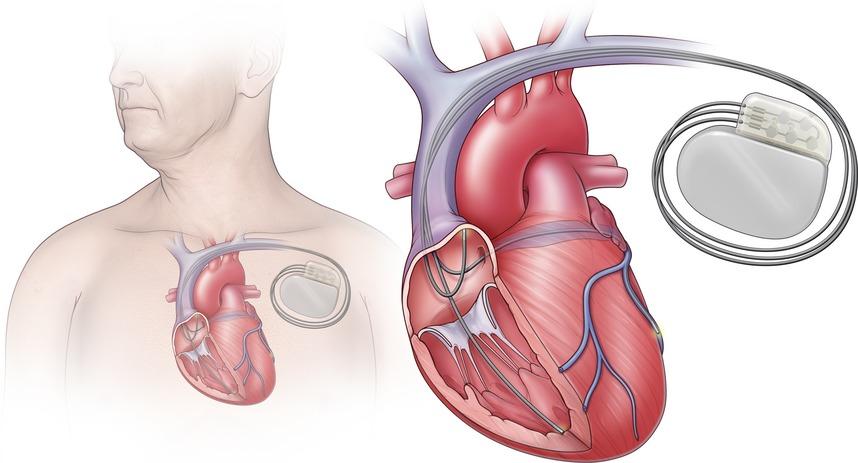
When people refer to a cardiac resynchronization therapy (CRT) device, they are discussing the system—the CRT device and the leads.
- A CRT device is a device implanted under the skin, typically just below the collarbone. The device delivers therapies to coordinate the heart’s pumping action and treats fast, irregular, or slow heart rhythms depending on the type of CRT device. This device may also be referred to as a heart failure device, a pacemaker for heart failure, a biventricular device, a three-lead CRT device, CRT-P (pacemaker), or CRT-D (defibrillator).
- Leads are thin, soft insulated wires about the size of a spaghetti noodle. The leads carry the electrical impulse from the CRT device to your heart and relay information about the heart’s activity back to the CRT device.
HOW DOES THE CRT WORK?
A cardiac resynchronisation therapy device monitors your heart rhythm 24 hours a day and sends electrical pulses to pace the lower chambers of your heart (ventricles) to help them beat in a more coordinated rhythm. This coordinating or “resynchronisation” therapy improves the heart’s ability to pump blood and oxygen more efficiently to the body. Your doctor will program the CRT device to deliver the most effective therapies for your specific heart condition.
In response to abnormal heart rhythms, a CRT device may also provide the following therapies:
- Pacing therapy for slow heart rhythms - electrical impulses are delivered to the heart when the heart’s own rhythm is too slow or irregular
- Defibrillation therapies for fast or irregular heart rhythms - a shock therapy is delivered to the heart to interrupt fast heart rhythms and restore a normal heart rate
There are two types of CRT devices—a CRT pacemaker (CRT-P) and a CRT defibrillator (CRT-D). CRT-D devices, like all defibrillators, have a pacemaker function in them. Both devices help to coordinate the heart’s pumping action and deliver pacing therapy for a slow heart rate. However, the CRT-D can also treat fast heart rhythms. All cardiac resynchronisation therapy devices are designed to use three leads. One lead is placed inside the right atrium, another lead is placed inside the right ventricle, and the third lead is placed inside a vein on the outside of the left ventricle.
THE CRT DEVICE BATTERY
The energy needed for the CRT to work comes from a battery inside the device. How long your battery lasts depends on several factors. Some of these factors include the type of CRT you have, the nature of your heart condition, and how often your CRT provides therapy to your heart. Because your CRT operates using a battery sealed inside the device, the entire device will need to be replaced when battery power falls to a low level. The leads only need to be changed in exceptional cases.
GETTING A CRT IMPLANTED
The procedure to implant a CRT does not require open heart surgery, and most people go home within 24 hours. Before the surgery, medication may be given to make you sleepy and comfortable. Generally, the procedure is performed under local anesthesia.
GENERAL STEPS OF AN IMPLANT PROCEDURE:
- A small incision, approximately 5 to 10 cm long, will be made in your upper chest area, just below your collarbone.
- Three leads will be guided through a vein into your heart, and the leads will be connected to the CRT device.
- The CRT device settings will be programmed, and the device will be tested to ensure it is working properly to meet your medical needs.
- The CRT device will be inserted beneath your skin, and the incision in your chest will be closed.
REPLACEMENT INTERVENTION
The CRT device has been developed to let your doctor know when the battery power falls to a low level. As the battery is an inherent component of the CRT device, the entire CRT device must be replaced during a replacement procedure. The surgeon makes an incision over the old scar and removes the old device. The electrodes are fastened securely and, after they have been checked, a new device is connected, tested and inserted into the existing skin pocket. The leads only need to be changed in exceptional cases.
REMOTE MONITORING OF YOUR CRT
We understand it is important to stay connected to your care team from the comfort of your home or wherever you’re traveling - remote monitoring allows for this flexibility.
Today, millions of people implanted with heart devices are remotely monitored.
Remote monitoring has been shown to:
- Communicate any heart rhythm and device changes which require attention
- Reduce hospitalizations and ER visits
- Increase Quality of Life
- Provide you with a sense of security and peace of mind

