
WHAT IS TACHYCARDIA?
Tachycardia is a condition where the heart beats too fast. A healthy heart beats 60 to 100 times per minute, pumping about 280 liters of blood every hour. Exercise, stress, or fear can cause the heart to beat faster, but this is a normal response. With tachycardia, the heart beats at more than 100 beats per minute and can beat as fast as 400 beats per minute for no specific reason. At this rate, the heart is not able to pump blood effectively to the body and brain.
There are different types of fast heart rhythms that can occur in either the upper chambers (atria) or lower chambers (ventricles) of the heart:
Atrial flutter and atrial fibrillation start in the upper chambers of the heart.
Ventricular tachycardia and ventricular fibrillation start in the lower chambers of the heart.
SYMPTOMS OF TACHYCARDIA
When your heart beats too fast, you may experience various symptoms, such as:
- Shortness of breath
- Dizziness
- Sudden weakness
- Fluttering in the chest
- Lightheadedness
- Fainting
![]()
![]()
![]()
![]()
![]()
CAUSES OF TACHYCARDIA
Tachycardia can occur for several reasons. Common causes of tachycardia include:
- Heart-related conditions such as high blood pressure (hypertension)
- Poor blood supply to the heart muscle due to coronary artery disease (atherosclerosis), heart valve disease, heart failure, heart muscle disease (cardiomyopathy), tumors, or infections
- Other medical conditions such as thyroid disease, certain lung diseases, electrolyte imbalance, and alcohol or drug abuse
- Emotional stress or drinking large amounts of alcoholic or caffeinated beverages
RISK FACTORS:
Certain conditions can increase your risk of developing an abnormally fast heartbeat (tachycardia), including:
- Coronary artery disease (atherosclerosis)
- Heart failure (poor pumping heart)
- Heart attack (myocardial infarction)
- Congenital heart defects (condition you are born with)
- Inflammatory or degenerative heart conditions
- Chronic lung disease
WHO IS AT RISK OF SUDDEN CARDIAC ARREST?
Generally, sudden cardiac arrest strikes without warning. People who are at a higher risk for SCA include:
- Those who have had a heart attack
- People who have heart failure
- Survivors of a previous SCA or those who have a family member who has had an SCA event
- People with a low ejection fraction (EF)
TREATING SUDDEN CARDIAC ARREST THROUGH DEFIBRILLATION
The most effective way to treat SCA is through defibrillation. Defibrillation involves delivering an electrical shock to your heart to restore a normal heartbeat.
There are two primary forms of defibrillation:
- An automated external defibrillator, or AED, is a portable device that is used by emergency response teams or the general public to shock the heart
- An implantable cardioverter defibrillator, or ICD, is a device that is implanted under the skin. The implantable cardioverter defibrillator delivers electrical pulses or shocks to treat fast, irregular rhythms.
WHAT IS AN ICD DEVICE?
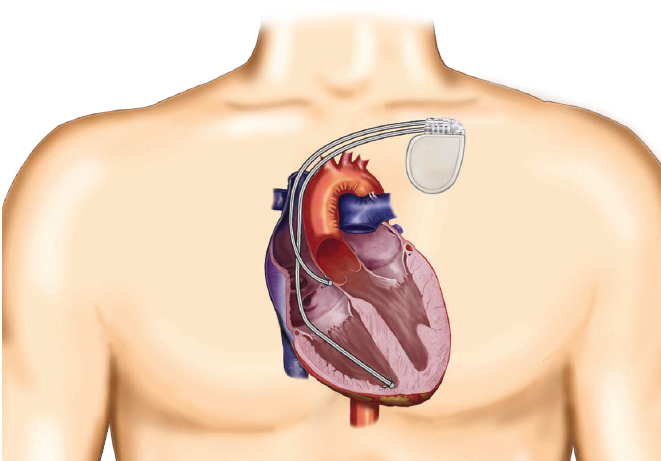
When people refer to an implantable cardioverter defibrillator, they are actually discussing the system - the defibrillator and the leads. A pulse generator (defibrillator) works like a small computer & continuously monitors the heart and automatically delivers electrical pulses or shocks to correct fast heart rhythms. It is a small device about the size of a matchbox and is usually inserted just under your collarbone.
Leads are thin soft insulated wires about the size of a spaghetti noodle. They are placed in your heart through a vein and are connected to the defibrillator. Leads carry the electrical impulse from the defibrillator to your heart and relay information about the heart’s natural activity back to the defibrillator.

HOW DOES THE ICD DEVICE WORK?
An implantable cardioverter defibrillator is designed to monitor your heart rhythm 24 hours a day. If your heart is beating too fast or irregularly, the device will first send small painless electrical signals to correct your heart rate (this is called anti-tachycardia pacing or ATP). If the fast heart rate (tachycardia) continues, the defibrillator will deliver an electric shock to restore your heart to a normal rate. This electric shock is synchronized with the heart’s rhythm as far as possible and is then referred to as cardioversion. If the electric shock cannot be synchronized with the heart’s rhythm, e.g. during ventricular fibrillation, it is referred to as defibrillation.
The implantable cardioverter defibrillator can also treat slow heart rhythms by sending electrical pulses to the heart to correct it.
Your doctor will program the ICD to deliver the most effective therapies for your specific heart condition.
THE ICD DEVICE BATTERY
The energy needed for the ICD to work comes from a special battery. How long your battery lasts depends on several factors. Some of these factors include the type of ICD you have, the nature of your heart condition, and how often your ICD provides therapy to your heart.
It could last up to 13 years. Because your ICD operates using a battery sealed inside the device, the entire device (pulse generator) will need to be replaced when battery power falls to a low level.
The leads only need to be changed in exceptional cases.
GETTING AN ICD IMPLANTED
The procedure to implant an ICD is minimally invasive, and most people go home within 24 hours. Before the surgery, medication may be given to make you sleepy and comfortable. Generally, the procedure is performed under local anesthesia.
GENERAL STEPS OF AN IMPLANT PROCEDURE:
A small incision, approximately 5 to 10cm long, will be made in your upper chest area, just below your collarbone.
One or two leads will be guided through a vein into your heart, and the leads will be connected to the implantable cardioverter defibrillator.
A single chamber ICD means you have one lead inserted into the lower right chamber (ventricle) of the heart.
A dual chamber ICD means that you also have a lead inserted into the upper right chamber (atrium) of the heart.
The defibrillator settings will be programmed, and the device will be tested to ensure it is working properly to meet your medical needs.
The pulse generator (defibrillator) will be inserted beneath your skin, and the incision in your chest will be closed.
After the procedure, you will be given an ICD identification card. Keep it with you at all times, as it contains important information about the implanted device.
REPLACEMENT PROCEDURE
The ICD has been developed to let your doctor know when the battery power falls to a low level. As the battery is an inherent component of the pulse generator, the entire pulse generator device must be replaced during a replacement procedure. The surgeon makes an incision over the old scar and removes the old device. The electrodes are fastened securely and, after they have been checked, a new pulse generator device is connected, tested, and inserted into the existing skin pocket. The leads only need to be changed in exceptional cases.
WHAT IS THE DIFFERENCE BETWEEN A TRADITIONAL ICD AND EV-ICD?
ICDs and EV-ICDs both have a defibrillator and a lead.
- The defibrillator functions like a small computer, continuously monitoring the heart and automatically delivering electrical pulses or shocks to correct fast heart rhythms. It is a small device about the size of a matchbox. A traditional ICD is inserted just under the collarbone, while the EV-ICD is inserted under the left armpit.
- The lead is a thin, soft, insulated wire, about the size of a spaghetti noodle, that transmits electrical signals from the heart to the defibrillator, allowing it to monitor the heart. The lead also delivers treatments from the defibrillator to the heart. With a traditional ICD device, the lead is placed in your heart through a vein. With an EV-ICD, the lead is placed under the sternum, outside the heart.
HOW DOES THE EV-ICD DEVICE WORK?
An EV-ICD is designed to monitor your heart rhythm 24 hours a day. If your heart beats too fast or irregularly, the device will first send small painless electrical signals to correct your heart rate.
This is called anti-tachycardia pacing or ATP. If the fast heart rhythm continues, the defibrillator will deliver an electric shock to restore your normal heart rhythm. This shock is referred to as cardioversion or defibrillation. The EV-ICD can also treat slow heart rhythms by sending electrical pulses to the heart to correct them. Your doctor will program the EV-ICD to provide the most effective therapies for your specific heart condition.
The energy required for the EV-ICD to work comes from a special battery. The battery life depends on several factors, including the nature of your heart condition and how often the EV-ICD delivers therapy to your heart.
The battery can last up to 10 years. Since the EV-ICD operates using a battery sealed inside the device, the entire device will need to be replaced when the battery power falls to a low level. The lead only needs to be replaced in exceptional cases.
HOW IS AN EV-ICD PUT IN?
A cardiologist (heart doctor) will put in your EV-ICD. You will be given a general anesthetic. You will have a chance to ask your care team questions and talk with them about any concerns and or fears.
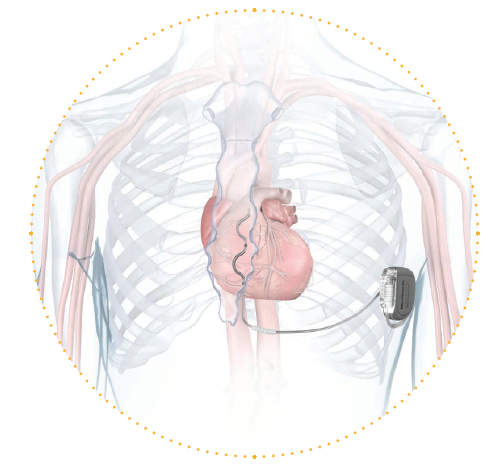
- Your surgeon makes a small cut just below the tip of your breast bone (sternum). The lead is pushed through this cut and into the space underneath your breast bone. The lead has curves in it to help keep it in place next to your heart.
- Once it is in place, the lead is tested to make sure it can accurately keep a check on your heart rate and send the right treatments.
- ΜNext, your surgeon makes a cut under your left armpit. A tool guides the free end of the lead out through the new cut so that the lead can be joined to the ICD.
- Your doctor sets up EV-ICD to give you the best treatment for your specific heart condition. The ICD is then placed under your skin and the cut is closed.
REPLACEMENT PROCEDURE
The EV-ICD is set up to let your doctor know when the battery power falls to a low level. When this happens, the whole ICD needs to be replaced as the battery is sealed inside it. To replace it, your surgeon makes a cut over the old scar and removes the old ICD. The lead is fastened securely to the new ICD and, after it has been checked, the new ICD is connected, tested, and put in place. The lead hardly ever needs to be changed.
REMOTE MONITORING OF ICD DEVICE
We understand it is important to stay connected to your care team from the comfort of your home or wherever you’re traveling - remote monitoring provides this flexibility.
Today, millions of people implanted with heart devices are remotely monitored. Remote monitoring has been shown to:
- Communicate any heart rhythm and device changes which require attention
- Reduce hospitalizations and ER visits
- Increase Quality of Life
- Provide you with a sense of security and peace of mind

